The cornea is the thin transparent tissue covering the front of the eye. The inner layer of cells, consisting of endothelial cells, are responsible for pumping fluid out of the cornea. In effect, this endothelial layer helps to keep the cornea crystal clear. Unfortunately, the endothelium does not regenerate. You are born with these cells and they do not grow back when they are damaged.

In certain eye conditions such as Fuch’s dystrophy and bullous keratopathy, the endothelial cells no longer function and this causes the cornea to swell and vision deteriorates as the cornea begins to cloud.
The usual thickness of the entire cornea is ~540 microns. When the endothelial cells are not pumping well, the cornea can swell to the 600-1000 micron range. The cornea is no longer clear when it is swollen because the collagen fibers are no longer able to remain parallel. At this point, the corneal dysfunction can usually be treated medically with saline eyedrops (Muro 128 Solution 5%, Bausch & Lomb or Sochlor 5% solution, OCuSOFT).
Swelling in the cornea, called corneal edema, can worsen to the point where blisters form in the cornea. These blisters can erupt causing painful bullae. This condition is called bullous keratopathy. Bullous means blisters and keratopathy means a disease of the cornea. At the point where the corneal swelling is no longer well controlled with medical therapy, we can turn to surgical treatments like DSEK.
How does the DSEK transplant work to keep the cornea clear?
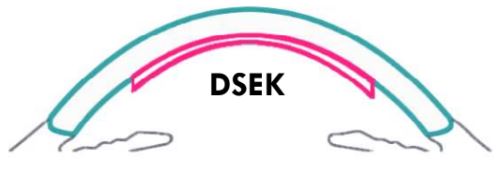
Descemet’s stripping automated endothelial keratoplasty (DSEK) is a type of partial thickness corneal transplant surgery. In this surgery, only the endothelial cell layer containing the endothelial cells and a very thin layer of cornea stroma are transplanted. The endothelial cells pump out fluid and keep the cornea clear. Meanwhile the thin cornea stroma provides a scaffold for the surgeon to transplant the cells.
During a DSEK corneal transplant, your cornea surgeon adds an additional 50-100 micron layer containing healthy endothelial cells which can pump the cornea to a clear and compact thickness. The cornea in addition to the transplanted tissue is now 600 – 700 microns thick, but the collagen fibrils in the graft and in the native cornea are now compact and parallel.
What is the difference between DSEK and DSAEK?
In the past the acronyms had different meanings:
DSEK: When the procedure was first starting out, surgeons would prepare the donor tissue with a manual dissection.
DSAEK: Is the automated version of the procedure where a microkeratome is used to precisely cut the tissue.
Nowadays, DSEK and DSAEK are used interchangeably to describe the same procedure using the microkeratome version. Surgeons in the recent past would prepare the tissue and cut it themselves in the operating room. Some skilled surgeons where I trained in the Cleveland Clinic still prepare their own tissues in the O.R. to this date. Mostly nowadays, to minimize operating room time, Eye Banks have taken over the tissue processing. Some eye banks even preload the tissue in cartridges allowing surgeons to streamline the surgery.
What is aftercare and recovery time like?
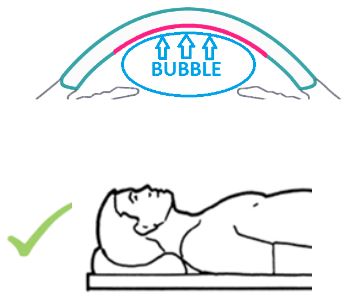
The DSEK graft is held into place with an air bubble which is placed in the eye. During the first 24 hours after surgery, position on our back facing upwards. Limit time upright to short trips to the bathroom and eating. Avoid looking downwards as that can cause the graft to detach and dislocate which requires additional procedures to reattach.
Your vision will be extremely blurry the first few days because the air bubble covering the graft will block out your vision. During the first few days, your surgeon may advise you to continue positioning on your back for several hours each day and to sleep directly on your backwards lookup at the ceiling. As the air bubble reabsorbs, you will notice a line in your vision. The bottom portion of your vision will be very blurry and the top portion will start to clear. As the bubble becomes smaller and smaller, you may notice it dance around as you walk or move from lying to standing.
Avoid rubbing or touching your eyes. Follow all post-operative instructions which usually include a series of drops and sometimes ointments. Typically, your surgeon will want to see you the day after surgery and within the first week of surgery. There are typically small nylon sutures which are placed in the surgical incisions that a removed 1 month after surgery. Typically, vision recovers by 1-3 months following surgery and continues to improve up to 2 years after surgery.
In higher risk surgeries like with patients who have a glaucoma drainage device or prior glaucoma surgery, it may be necessary to return to the operating room or procedure room for a rebubble procedure in which your surgeon places more air into the eye to allow the corneal graft to completely attach. Each surgeon is different, but after the 3-month post-operative check, I then like to see my patients every 6 months to check on the health of the graft.
This article was originally written on 6/20/2022 by Angelique Pillar, MD and updated on 5/28/23.
